Labour and vaginal birth
The three stages of labour

The first stage
The first stage begins with the onset of regular contractions and ends when the cervix is fully dilated.
Early labour: cervical effacement (thinning out) and dilatation. The experience of labour varies widely, but typically contractions start every ten minutes lasting 30 seconds each.
Eventually they become every five minutes lasting 40 to 60 seconds as you reach the end of early labour. Early labour contractions can be painful but you will find you can still talk through them and putter around the house.
You may want to go for a walk or relax instead, take a warm bath, watch a video, or doze off between contractions if you can. Increasing vaginal mucousy discharge which may be tinged with blood is called the “show” and is normal.
Early labour ends when your cervix is 3cm dilated at which point you start making more progress. It is not easy to tell how long early labour lasts and when true labour starts because early labour contractions are hard to distinguish from inefficient Braxton Hicks contractions.
Don’t become a slave to your stopwatch,
Stay rested, Stay hydrated, Drink lots.
Active/true labour: Rapid dilatation of the cervix, stronger longer contractions. This is the time when things really start happening. In contrast to early labour, you’ll no longer be able to talk through the contractions.
As a general rule, once you’ve had regular, painful contractions (each lasting about 60 seconds) every five minutes for an hour, it’s time to call us and head to the hospital. In most cases, the frequency of contractions eventually increases to every two-and-a-half to three minutes, although some women may never have them more often than every five minutes.
Labour and delivery in first time mothers can take an average of 15 hours. For women who have laboured before, labour averages around eight hours
Breathe, Relax, Get massaged, Walk around.
Transition is the last part of active labour, when you cervix goes from 8 to 10 cm. It is intense, contractions are strong, your baby descends. You may feel rectal pressure, have a bloody discharge and feel very nauseated. Transition can take a few minutes or a few hours
Don’t lose hope, The end is near!
The second stage
The second stage of labour begins with full dilatation and ends with the birth of your baby. This is often referred to as the pushing stage. You will feel the urge to push as your baby’s head descends.
With each contraction, the force of your uterus — combined with the force of your abdominal muscles if you’re actively pushing — exerts pressure on your baby to continue to move down through the birth canal. It is not unusual to try different positions.
As your baby gets closer to your perineum, the urge to push is compelling, the pressure on your perineum intense. Crowning is when the widest part of baby’s head is visible, followed by head, shoulders and body.
The cord will be clamped and cut. If all is well, your baby will be lifted onto your bare belly so you can touch, kiss, and simply marvel at him. The skin-to-skin contact will keep your baby nice and toasty, and he’ll be covered with a warm towel.
The third stage
The third and final stage begins right after the birth of your baby and involves the separation and delivery of the placenta. This stage is not difficult or painful and can last up to 30 minutes. By now your focus has shifted to your baby, and you may be oblivious to everything else going on around you.

Monitoring your baby during labour
Reasons for monitoring your baby:
- Labour can be a stressful time for babies as well as mothers. Some babies don’t cope well, especially if they are small or already compromised in some other way.
- Guidelines issued in 2001 by the National Institute for Clinical Excellence (NICE) recommend that women with uncomplicated pregnancies can be monitored at regular intervals using intermittent auscultation. Women with high risk pregnancies require continuous electronic foetal monitoring (EFM)
You can read this in more detail at www.nice.org.uk
Types of monitoring:
- Intermittent monitoring with a sonicaid during labour is done every fifteen minutes during the first stage of labour, and once every five minutes during the pushing stage.
- Continuous electronic foetal monitoring (EFM) is done with two sensors on your tummy held in place by elastic belts. They monitor your baby’s heart beat and your contractions, and are recorded on paper. Sometimes monitoring is done via a foetal scalp electrode on your baby’s head and this provides a more accurate reading.
Continuous monitoring is advisable in the following situations:
- Induction of labour
- Use of epidural pain relief
- Labour before 37 weeks of pregnancy (preterm)
- Labour after 40 weeks of pregnancy (overdue)
- Suspicious bleeding in late pregnancy or during labour
- Previous caesarean section
- A small baby
- Pre-eclampsia
- Diabetes
- Heart disease
- Twins or triplets

Fetal blood sampling
 Electronic readings can be difficult to interpret. If the reading looks suspicious, sometimes a tiny sample of blood will be taken from you baby’s scalp. This provides more accurate information on how well your baby is coping with labour. The procedure is not painful and is done usually with you lying on your back or side.
Electronic readings can be difficult to interpret. If the reading looks suspicious, sometimes a tiny sample of blood will be taken from you baby’s scalp. This provides more accurate information on how well your baby is coping with labour. The procedure is not painful and is done usually with you lying on your back or side.
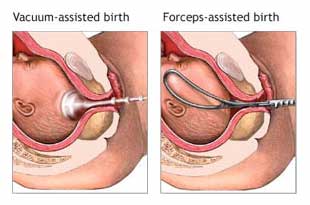
Assisted delivery (forceps and ventouse)
An assisted delivery is when either forceps or ventouse are used to help your baby be born.
The choice of instrument depends on many factors, and your Birthright obstetrician will discuss the best choice for you and your baby
If an assisted delivery becomes necessary, your legs will often be placed in supports at the side of the bed (the lithotomy position) and the end of the bed removed. Your bladder will be emptied with a catheter. Pain relief will be given. Often an episiotomy is necessary. An assisted delivery is a combined effort with your doctor pulling gently and you pushing to help your baby through. Often a paediatrician will be present.
Forceps are sometimes described as ‘stainless steel salad servers’ or ‘large sugar-tongs’. They come in two intersecting parts, and have curved ends to cradle the baby’s head. There may be some bruising where the blades have been applied but this is temporary.
The ventouse has a cup attached to a small vacuum pump. The cup, which fits on top and slightly towards the back of your baby’s head, may be made of metal or silicone plastic. The type of cup used may depend on your baby’s position. There may be some bruising and your baby may have a cone shaped head for a day or so.
Reasons for an assisted delivery:
Foetal distress: if your baby becomes distressed during the second (pushing) stage of labour
- If you are exhausted
- If your baby is in a difficult position
- If your baby isn’t making any progress through your pelvis despite valiant pushing
- If there’s a medical reason why you shouldn’t push for too long (e.g. heart disease)
- If you have twins or triplets, you are more likely to need an assisted delivery particularly for the second baby

Our goal at Birthright is to provide you the best gynaecological care in a friendly and relaxed atmosphere, where you can talk to us about your needs.
Call us and discuss your care.
0800 247 848
